 Limited Edition Golden Llama is here! Check out how you can get one.
Limited Edition Golden Llama is here! Check out how you can get one.  Limited Edition Golden Llama is here! Check out how you can get one.
Limited Edition Golden Llama is here! Check out how you can get one.
 Offering SPR-BLI Services - Proteins provided for free!
Offering SPR-BLI Services - Proteins provided for free! Get your ComboX free sample to test now!
Get your ComboX free sample to test now!
 Time Limited Offer: Welcome Gift for New Customers !
Time Limited Offer: Welcome Gift for New Customers !  Shipping Price Reduction for EU Regions
Shipping Price Reduction for EU Regions
> Insights > The Top Risk of CAR-T Therapy: Cytokine Release Syndrome (CRS) ——Assessment, grading and management of CRS CAR-T cell therapy brings the hope of a cure to many cancer patients. Despite the outstanding effectiveness, the toxicity called cytokine release syndrome (CRS) has drawn more and more attention.
In this article it is aimed to summarize the key points of assessment, grading and management of CRS in CAR-T Therapy, and the answers to the following questions will be cleared after reading the text:
• How to identify the onset of CRS clinically?
• What is the CRS management?
• What is the ASTCT CRS consensus grading?
• How to use tocilizumab in CRS management?
Assessment, grading and managment of CRS in CAR-T therapy
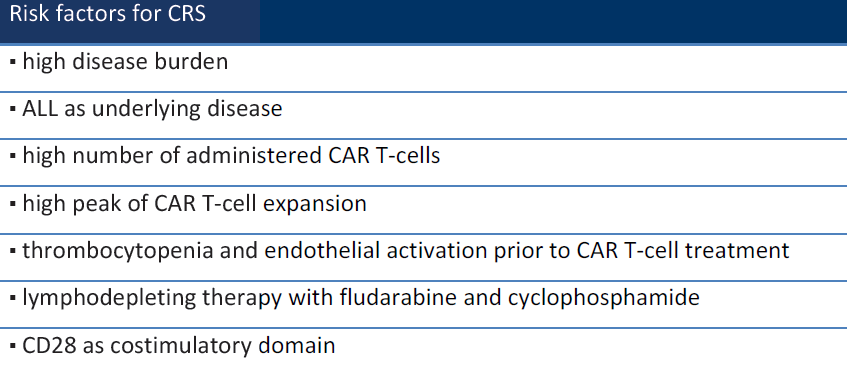
In recent years, CAR-T cell therapy brings the hope of a cure to many cancer patients. Despite the outstanding effectiveness, the toxicity called cytokine release syndrome (CRS) is a severe problem. After the infusion of CAR-T into the human body, T lymphocytes are activated and proliferate rapidly, causing the excessive release of cytokines including TNF-α, IFN-γ, IL-1, IL-2, IL-4, IL-6, IL-8, IL-10, and IL-12. Fever, hypotension, myalgia, blood coagulation disorders, dyspnea, and end-organ dysfunction are possible outcomes. These may cause permanent damage to tissues and organs or even cause death. In short, CRS is an acute systemic inflammatory syndrome that is associated with CAR-T cell therapy [1]. However, many factors can affect the chance to have CRS, including disease state, treatment procedure, and drugs [2]. (Table 1)
Table 1 Risk factors for CRS
How to identify the onset of CRS clinically? CRS patients usually have elevated levels of serum CRP and ferritin. They can be used as biomarkers to determine the occurrence of CRS. But all these markers, including ferritin, CRP, LDH, AST, ALT, and creatinine appear only after the clinical manifestations of CRS. We are not able to know the onset of CRS through them. Most hospitals cannot monitor real-time cytokine levels. Instead, they can only observe the clinical manifestations. Factors such as the type of CAR-T therapy and the patient's disease state usually decide when the CRS is going to happen. For patients using Kymriah, which contains the costimulatory domain of 4-1BB (CD137), the CRS peaks on the 3rd and 7th day after the administration. However, for patients using Yescarta or Tecartus, which contain the costimulatory domain of CD28, the CRS happens earlier on the second day of administration. But some delayed CRS were reported after 3 weeks of CAR-T administration as well [2].
In 2019, the American Society for Transplantation and Cell Therapy (ASTCT) developed a CRS consensus grading guideline (Table 2). According to the guideline, fever (≥38°C) is a requirement. With or without hypotension and/or hypoxia, the conditions get severer. Studies have shown that the ASTCT grading system can provide an objective, accurate, and repeatable rapid assessment of the severity of CRS clinically [2-3].
Table 2 ASTCT CRS Consensus Grading
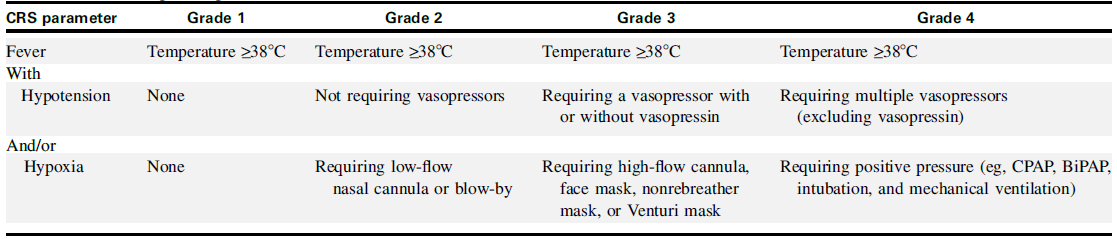
Grade 1) CRS patients with fever and some non-specific signs but no hypotension or hypoxia are classified into grade 1. The treatment strategy is the intravenous infusion of antipyretic drugs.
Grade 2) They define grade 2 CRS as fever (≥38.0°C) with hypotension not requiring vasopressors and/or hypoxia requiring the use of oxygen delivered by low-flow nasal cannula (≤6 L/minute) or blow-by. But it is important to note that CRS patients are at risk of edema due to vasodilatation and capillary leakage. Therefore, fluid infusion needs to be closely monitored. Tocilizumab, which inhibits IL-6, can be used for grade 2 patients. Studies have shown that early use of tocilizumab can reduce the incidence of severe CRS and organ failure while preserving the efficacy of CAR-T therapy.
Grade 3) For patients with Grade 3 CRS, that is, patients with fever, low blood pressure and no response to fluid infusion, and patients who require high flow oxygen (≥6L/min), they should consider entering the intensive care unit (ICU) for management and use care Belizumab and glucocorticoids (dexamethasone, etc.) for treatment. To prevent further deterioration and visceral damage, it is recommended to use vasopressor (such as norepinephrine) and/ or high-flow nasal cannula (>6 L/minute). Besides, high-grade CRS patients are prone to cardiac dysfunction, it is recommended to closely monitor their cardiac function.
Grade 4) We define grade 4 CRS as fever (≥38.0°C) with hypotension requiring multiple vasopressors (excluding vasopressin) and/or hypoxia requiring positive pressure (eg, CPAP, bilevel positive airway pressure, intubation, mechanical ventilation) not attributable to any other cause. In addition to the treatment for grade 3 CRS, methylprednisolone is recommended to use at a dose of 1g/day. Studies have shown that high-grade CRS is reversible through early intervention.
Roche's tocilizumab (trade name: Actemra) is a drug approved by the FDA in 2017. It was designed for the CRS caused by CAR-T therapy through the blockage of the inflammatory cytokine interleukin-6 (IL -6).
Some clinical guidance of tocilizumab [4]:
(1) For elderly patients or patients with severe complications, tocilizumab should be considered in the early stage of CRS.
(2) Tocilizumab can be administered for adults with grade 2 CRS, and children with grade 3 CRS.
(3) Tocilizumab can be administered to pediatric patients who develop grade 2 CRS, but intolerant to fever.
(4) For adults and children administered one dose of tocilizumab, if the conditions do not improve, the second dose should be together with glucocorticoids. If the condition is still not improved, Anakinra, Siltuximab, and a high dose of methylprednisolone should be considered.
Researchers are working hard to avoid or treat CRS. In 2018 on the same day, Nature published two articles about a new way to control CAR-T toxicity. Their research proved that the inhibition of IL-1 reduces the macrophage induced CRS. In 2019, Michel Sadelain, director of the Cell Engineering Center of Sloan Kettering Cancer Center, published an article in Science translational medicine. He identified a functional switch in CAR-T cells helping to avoid CRS in mouse models [5]. In January 2020, a research team from the Chinese Academy of Medical Sciences published an article in Science Immunology. This article talked about the process of pyrolysis caused by CAR-T therapies, and the mechanism of CRS. From their clear microscope images, we can see the whole process of CRS triggered by CAR-T cell therapy [6]. With the continuous clinical research of CAR-T therapies and CRS, we can expect breakthroughs soon.
ACROBiosystems developed a series of CAR-T target proteins, including CD19, BCMA, CD22 MSLN, and EGFR. We have all these proteins in different forms like non-labeled, biotin-labeled and fluorescent-labeled, etc. We also provide the flow cytometry protocols for CAR expression detection.
ACRO FITC-labeled CD19 protein (Cat. No. CD9-HF2H2) is highly specific and sensitive in anti-CD19 CAR detection assays. Besides, we developed another antibody (Cat. No. FM3-FY45) targeting the antigen-binding epitope of FMC63 scFv. This product provides an additional method for Anti-CD19 (FMC63) CAR detection.
ACRO FITC-labeled BCMA protein (Cat. No. BCA-HF254) brings good sensitivity. This product has been widely used in different assays and is well recognized in the industry.
Product list
CD19
BCMA
Anti-FMC63 mAb
Case study
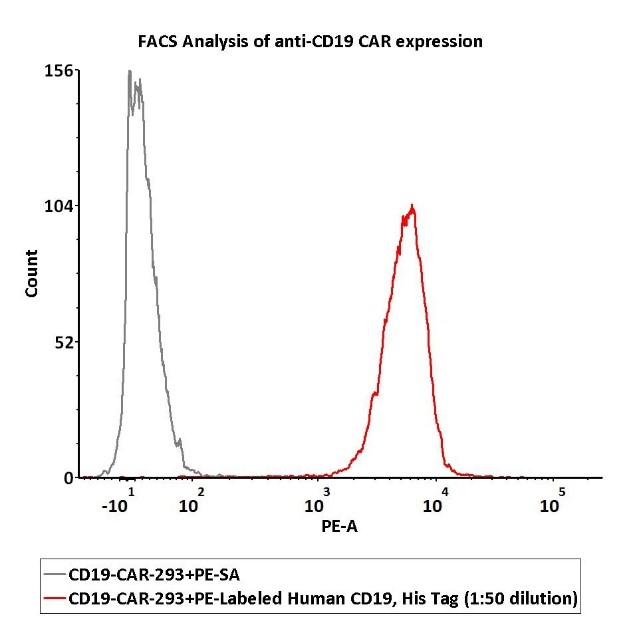
1e6 of the anti-CD19 CAR-293 cells were stained with 100 μL of 1:50 dilution (2 μL stock solution in 100 μL FACS buffer) of PE-Labeled Human CD19 (20-291), His Tag (Cat. No. CD9-HP2H3). PE Streptavidin was used as negative control.
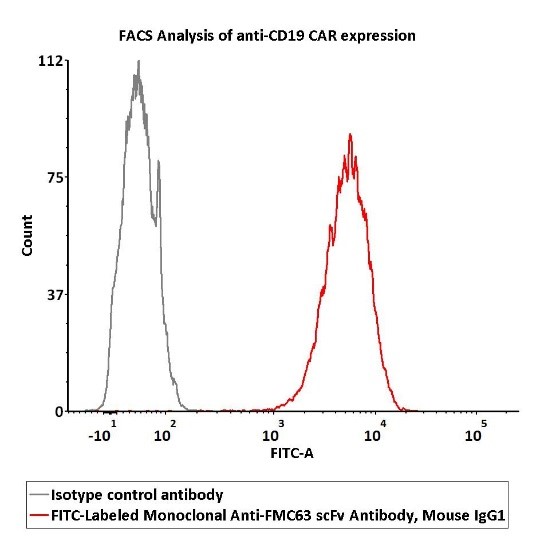
2e5 of Anti-CD19 CAR-293 cells were stained with 100 μL of 1:50 dilution (2 μL stock solution in 100 μL FACS buffer) FITC-Labeled Monoclonal Anti-FMC63 scFv Antibody, Mouse IgG1 (Cat. No. FM3-FY45) and isotype control respectively. FITC signal was used to evaluate the binding activity.
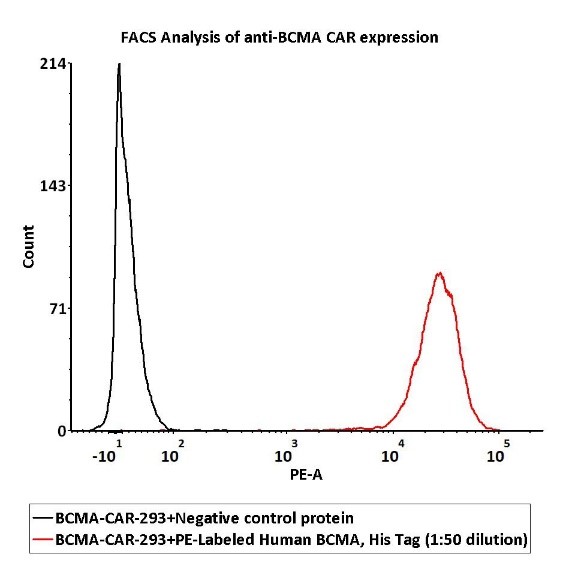
1e6 of the Anti-BCMA CAR-293 cells were stained with 100 μL of 1:50 dilution (2 μL stock solution in 100 μL FACS buffer) of PE-Labeled Human BCMA Protein, His Tag (Cat. No. BCA-HP2H2) and negative control protein respectively, PE signal was used to evaluate the binding activity.
References:
[1] https://www.cn-healthcare.com/articlewm/20190306/content-1047067.html.
[2] Schubert ML, Schmitt M, Wang L, et al. Side-effect management of chimeric antigen receptor (CAR) T-cell therapy. Ann Oncol. 2021;32(1):34-48.
[3] Freyer CW, Porter DL. Cytokine release syndrome and neurotoxicity following CAR T-cell therapy for hematologic malignancies. J Allergy Clin Immunol. 2020;146(5):940-948.
[4] Maus MV, Alexander S, Bishop MR, et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immune effector cell-related adverse events. J Immunother Cancer. 2020;8(2):e001511.
[5] Mestermann, Katrin, et al. "The tyrosine kinase inhibitor dasatinib acts as a pharmacologic on/off switch for CAR T cells." Science translational medicine 11.499 (2019).
[6] Liu, Yuying, et al. "Gasdermin E–mediated target cell pyroptosis by CAR T cells triggers cytokine release syndrome." Science immunology 5.43 (2020).
This web search service is supported by Google Inc.
